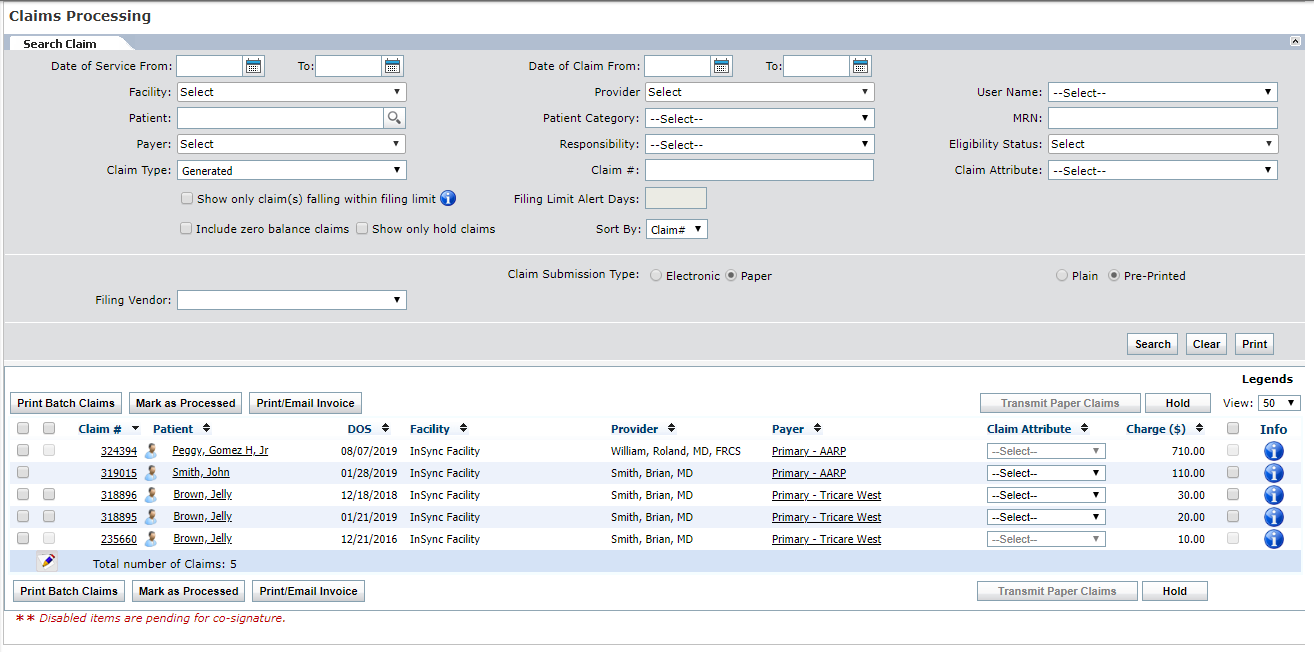
Claims Processing
Once claims are generated, you can submit from Billing > Claims Processing.
Once in the Claims Processing queue, users can search for individual claims by Date of Service, Facility, Provider, Patient Name, Patient Category, Payer, User Name, Responsibility, Supervising Provider, Claim Attribute, Claim Number, Financial Class, Claim Type, Filing Vendor, Error Severity, Billing Entity, Billing Type, and Submission Type.
The system is defaulted to display all new, electronic claims, with a default view of 50 results per page. Click on the blue heading link to sort by that heading.
Claims can be further filtered by Submission Type (paper or electronic). Use the Submission Type radial button to toggle between the Electronic and Paper queues.
You can also print encounter notes while printing claims from the Claims Processing screen. To do this, select the check box that appears prior to the claim number while printing claims. You can view the encounter note after closing the claim preview screen.
Clicking on different underlined parts of the claim listing will bring the user to the following screens:
| • | Patient Name – Patient Demographics |
| • | Claim # – Claim Details |
| • | Payer – Insurance Details |
See also, |